
Vitamin D Testing
Vitamin D is often referred to as the "sunshine vitamin" because its main source is sun exposure. However, it can also be found in cod liver oil, fatty fish (such as salmon, mackerel, and tuna), egg yolks, and foods that have been fortified with Vitamin D (milk, soy milk, orange juice, cereal, and oatmeal).
Vitamin D is fat-soluble, and our bodies produce the inactive form in our skin after exposure to sunlight (UVB rays). The inactive form (from skin production or diet) undergoes two transformations, with the first in the liver and the second in the kidneys to become the active form Vitamin D. However, the production of Vitamin D in our skin can be affected by a few different factors:
Sunscreens - They absorb the solar UVB rays, preventing Vitamin D production in the skin
Skin pigmentation - Individuals with more melanin (darker skin) also produce less Vitamin D. It takes as much as 6 times longer to produce the same amount of Vitamin D as someone with less pigmentation.
Age - Decreases with age due to diminished ability to produce it in the skin and also normal age related declines in kidney function.
Digestive Dysfunction - lack of absorption from the diet in people who have digestive issues like Crohn's, Ulcerative colitis and Food sensitivities.
Kidney Function - Kidney function decreases with age and so we lose our ability to convert to the active form with normal aging. This would also be decreased in anyone with kidney disease or kidney function issues.
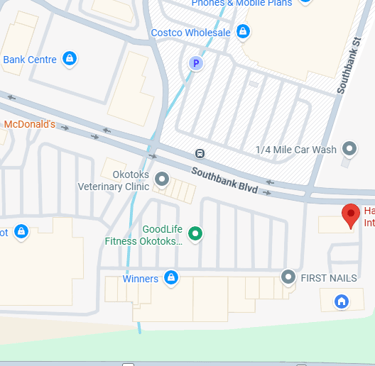
Zenith Angle (angle of the sun from the horizon) - It increases during the winter, in the early morning and later afternoon which increases the path that UVB rays have to pass through the ozone layer before they can be absorbed. When you live above or below 33 degrees latitude from the equator, very little Vitamin D is made in the skin. This means that Vitamin D is only produced in the skin from 10 am to 3 pm in the summer. It is estimated that in Alberta, you do not produce Vitamin D for a minimum of 6 months, regardless of how sunny the winter days are or the fact we see over 300 days of sun a year.
What role does Vitamin D play in our health?
Promotes calcium absorption in the digestive system to maintain serum calcium and phosphorus levels
Metabolic function
Bone growth and remodelling
Immune function
Glucose metabolism
Neuromuscular function
Cell growth
Reduction of inflammation
Pregnancy and Vitamin D
Low prenatal and neonatal Vitamin D levels may increase the susceptibility to:
Schizophrenia
Type 1 Diabetes
Multiple Sclerosis later in life
Increased risk for preeclampsia
Gestational diabetes
Preterm birth
Small size for gestational size.
Having optimum levels of Vitamin D has been found to
Prevents deadly cancers
Reduces the risk of diabetes
Prevent cognitive decline
Decrease depression
Reduce pregnancy complications
Decrease allergies
What can a Vitamin D deficiency do?
Vitamin D has a role in a variety of diseases and health conditions. Here are some of the most common deficiencies:
References:
Agmon-Levin, N., Theodor, E., Segal, R. M., & Shoenfeld, Y. (2013). Vitamin D in systemic and organ-specific autoimmune diseases. Clinical reviews in allergy & immunology, 45(2), 256–266. https://doi.org/10.1007/s12016-012-8342-y
Cigolini, M., Iagulli, M. P., Miconi, V., Galiotto, M., Lombardi, S., & Targher, G. (2006). Serum 25-hydroxyvitamin D3 concentrations and prevalence of cardiovascular disease among type 2 diabetic patients. Diabetes care, 29(3), 722–724. https://doi.org/10.2337/diacare.29.03.06.dc05-2148
Holick M. F. (2004). Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. The American journal of clinical nutrition, 80(6 Suppl), 1678S–88S. https://doi.org/10.1093/ajcn/80.6.1678S
Holick M. F. (2008). Vitamin D and sunlight: strategies for cancer prevention and other health benefits. Clinical journal of the American Society of Nephrology : CJASN, 3(5), 1548–1554. https://doi.org/10.2215/CJN.01350308
Hossein-nezhad, A., & Holick, M. F. (2013). Vitamin D for health: a global perspective. Mayo Clinic proceedings, 88(7), 720–755. https://doi.org/10.1016/j.mayocp.2013.05.011
Mathieu C, Badenhoop K. Vitamin D and type 1 diabetes mellitus: state of the art. Trends Endocrinol Metab. 2005;16(6):261-266. doi:10.1016/j.tem.2005.06.004
Pilz, S., Tomaschitz, A., März, W., Drechsler, C., Ritz, E., Zittermann, A., Cavalier, E., Pieber, T. R., Lappe, J. M., Grant, W. B., Holick, M. F., & Dekker, J. M. (2011). Vitamin D, cardiovascular disease and mortality. Clinical endocrinology, 75(5), 575–584. https://doi.org/10.1111/j.1365-2265.2011.04147.x
Schwalfenberg, G. K., Genuis, S. J., & Hiltz, M. N. (2010). Addressing vitamin D deficiency in Canada: a public health innovation whose time has come. Public health, 124(6), 350–359. https://doi.org/10.1016/j.puhe.2010.03.003
van Groningen, L., Opdenoordt, S., van Sorge, A., Telting, D., Giesen, A., & de Boer, H. (2010). Cholecalciferol loading dose guideline for vitamin D-deficient adults. European journal of endocrinology, 162(4), 805–811. https://doi.org/10.1530/EJE-09-0932
Wang, H., Chen, W., Li, D., Yin, X., Zhang, X., Olsen, N., & Zheng, S. G. (2017). Vitamin D and Chronic Diseases. Aging and disease, 8(3), 346–353. https://doi.org/10.14336/AD.2016.1021
Wei, S. Q., Qi, H. P., Luo, Z. C., & Fraser, W. D. (2013). Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 26(9), 889–899. https://doi.org/10.3109/14767058.2013.765849
Ricketts in Children
Osteomalacia
Osteoporosis
Autoimmune conditions (Systemic Lupus Erythematosus (SLE), Rheumatoid Arthritis, Multiple Sclerosis (MS), Diabetes
Primary biliary cirrhosis
Metabolic syndrome
Insulin resistance
Cardiovascular disease
Periodontitis
Preeclampsia
Schizophrenia
Immune system regulation
Inflammation
Alzheimer's
Epilepsy
Neurocognitive decline
Dementia
Increased fracture risk
Chronic liver disease
Chronic Hepatitis C
Non-alcoholic fatty liver disease
Psoriasis
Osteoarthritis
Chronic kidney disease
How much Vitamin D to take?
In 2010, it was estimated that 70-97% of Canadians are Vitamin D deficient. It has been harder to get a more recent estimate, as many health regions in Canada no longer test for Vitamin D levels. It is assumed that everyone is deficient and needs to supplement it. The best way to determine how much you need to take is by testing and determining your vitamin levels.
Once you have your blood vitamin D levels, Alberta Precision Laboratories provides the following interpretation:
Severe deficiency = <25.0 nmol/L
Moderation to Mild deficiency = 25.0 - 80.0 nmol/L
Optimum levels = 80.0 - 200.0 nmol/L
Toxicity possible = >250.0 nmol/L
Taking high doses of Vitamin D can lead to toxic levels, as it is a fat-soluble vitamin, which means your body will retain it rather than excreting the excess (like Vitamin C). As most Canadians are deficient, it does take months to years of dosing at very high levels to reach the toxicity range. Health Canada lists the upper tolerable limit now at 2,500 IU daily, but research has found that Vitamin D is weight-dependent.
It is best to talk to your doctor or health care provider to have your Vitamin D levels tested regularly to determine your personalized dose. The optimum range is based on your personal health history and health conditions to determine where in that range you need to be.
Book now to find out where your Vitamin D levels are and how much you need to take orally or to discuss Vitamin D injections with Dr. Kaler, ND
This website is for educational purposes only. The content on this website is not meant to treat, diagnose or prevent any conditions. Always consult with a qualified healthcare provider for your care. The author of this website is not liable for any adverse effects that may occur based on any information obtained here. Copyright ©2013-2025 by Harmony Health Integrative Centre. All Rights Reserved
GET IN TOUCH

HOURS
MONDAY TO FRIDAY
10 am to 6 pm
SATURDAY
By Appointment Only
SUNDAY / HOLIDAYS
Closed
CLOSURES
December 22, 2025
to January 5, 2026 February 17, 2026 April 18, 2026 May 19, 2026 July 1, 2026 August 4, 2026
